CALIFORNIA—As COVID-19 cases continue to climb across the state, averaging 40,000 new daily cases in the week before Christmas, Governor Gavin Newsom unveiled a plan to partner with pharmacies beginning Monday, December 27, to vaccinate residents and staff at nursing homes and assisted living facilities. The partnership between the Centers of Disease Control and pharmacies is formally known as the Pharmacy Partnership for Long-Term Care Program.
During a press conference, Newsom said the federal partnership with CVS and Walgreens began vaccinating the “most vulnerable Californians” on Monday. In phase one of the program, CVS will provide vaccinations for 499 skilled nursing facilities. Walgreens will do the vaccinations for 357 facilities. Newsom pointed out that since October 1, 65 percent of ICU admissions and 80 percent of deaths are in the 61 or older group.
Governor Newsom said that it was critical to vaccinate those most vulnerable to COVID, particularly in nursing homes. “By leveraging CVS and Walgreens resources, we can effectively deploy vaccines to residents and staff at our long-term care facilities, which are at higher risk of COVID transmission – and do it at no cost to the state or local government.”
Nursing homes have been a focal point of COVID deaths, and according to studies by the California Department of Public Health, account for 35 percent of California COVID deaths, despite only accounting for 5 percent of the state’s cases.
Plan 1 of the Pharmacy Partnership for Long-Term Care Program includes parts A and B. The Pfizer-BioNTech vaccines, approved on December 11 by the Food and Drug Administration, will be sent directly to the pharmacies. The skilled nursing homes, included in part A, are being vaccinated first. In part B, the assisted living facilities, residential care, and other long-term care facilities.

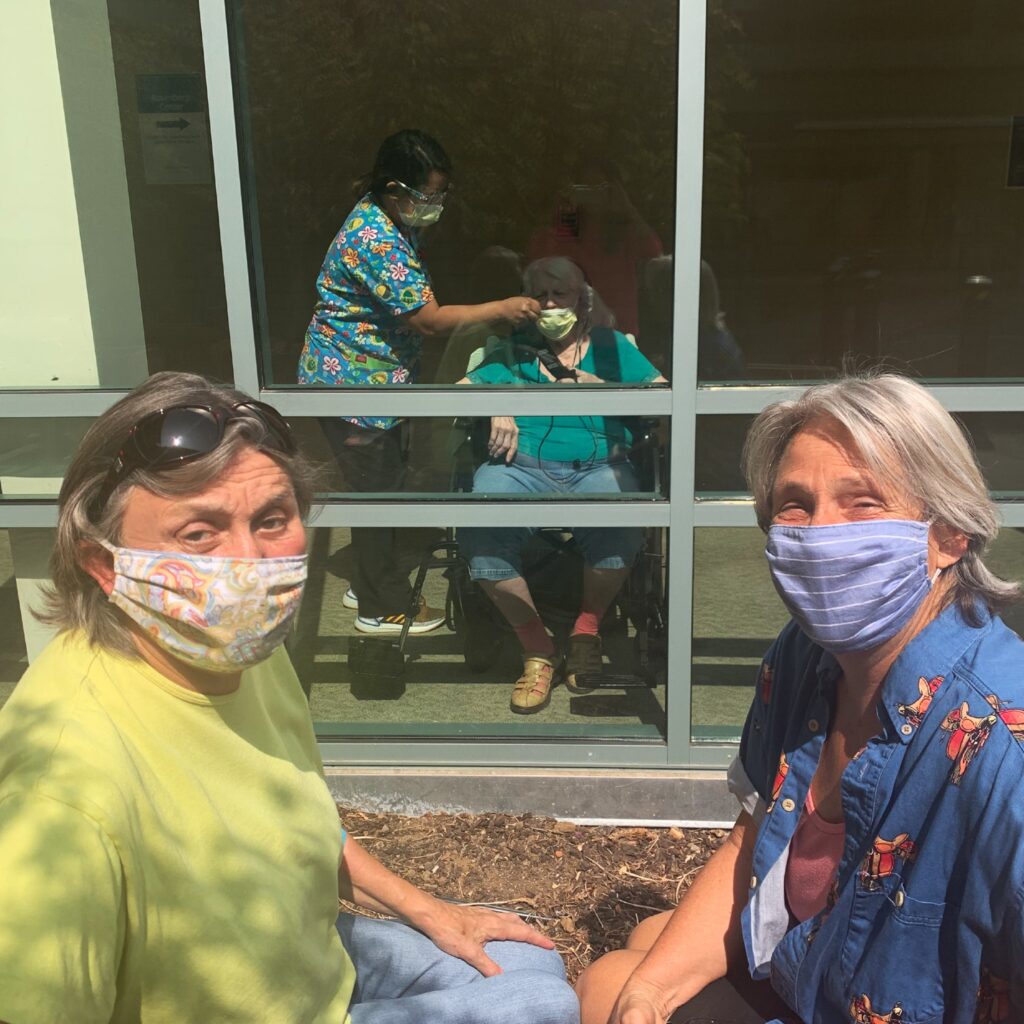
Photo by Sara Shaffer/Shared via UCSF Box.
The vaccines will be administered at the nursing homes and assisted living facilities. Pharmacy staff will visit each facility multiple times to ensure that all residents and staff who wish to be vaccinated get the vaccine. Phase A activities are estimated to take 3-4 weeks.
CVS announced that the pharmacy chain has the capacity to immunize close to 700,000 residents and staff across more than 15,000 skilled nursing and assisted living facilities in California.
In a CVS Health press release from December 21, pharmacy teams administered the first dose of the vaccine in facilities across 12 states during the week of the release, and the company expects to vaccinate up to 4 million residents and staff in 40,000 facilities throughout those states. The pharmacy chain will have the capacity to administer 20 to 25 million shots per month.

The care facility vaccination plan is a precursor to the plan of COVID-19 vaccine availability at pharmacies to the public in a retail setting. In that retail setting, vaccines are free and will be offered on an appointment-only basis on CVS.com or through the CVS Pharmacy app.
Walgreens is following the CDC’s phased distribution schedule to administer the COVID-19 vaccination. Phase 1a healthcare workers, residents of long-term care facilities, and selected populations based on guidelines. Phase 1b includes persons aged 75+, certain groups of healthcare workers. Phase 1c includes persons aged 65-74, persons aged 16-64 with chronic health conditions, and certain groups of essential workers. Phase 2’s goal is to make the vaccine accessible to the public in a retail space by the Spring of 2021.
“The long-term care facilities had an opportunity either to use CVS or Walgreens. Or they could have opted out and used a state program,” said CVS Health Bay Area regional director Joe Fiesel, as quoted on the Marin County Human Health Services website.
In Los Angeles County, the hardest hit region in California, all but the cities of Long Beach and Pasadena, are not included in this partnership with the pharmacies. As of December 29, there is on average, one COVID death every ten minutes in Los Angeles.
In San Francisco County, as of December 30, the San Francisco Campus for Jewish Living, Jewish Home & Rehab Center, reported 73 cases and less than 11 deaths among residents, and 50 cases among staff. The Laguna Honda Rehabilitation Center reported 41 cases and less than 11 deaths among residents, and 119 cases among staff. Buena Vista Manor House, a retirement home reported 25 COVID cases and less than 11 deaths among residents, and 13 cases among staff. Providence Palace, an assisted living facility also had roughly the same number of cases among residents as Buena Vista Manor House according to data published by the Los Angeles Times.
The Alden Terrace Convalescent Hospital, a skilled nursing facility impacted in Los Angeles County, reported 136 cases and 30 deaths among residents, and 46 cases among staff. At the Alameda Care Center, 87 cases and 26 deaths were reported among residents, and 49 cases and at least 11 deaths were reported among staff.
Aware of the dilemma at nursing homes, Interim California State Public Health Officer Dr. Erica Pan said, “This partnership is an opportunity to augment other vaccination efforts at the local level to prioritize our most vulnerable Californians where we are seeing the most outbreaks, hospitalizations, and deaths,” said Dr. Pan. “The partnership also allows us to continue to vaccinate other high priority individuals such as our front-line health care workers who are critical to our ongoing response to a surge of cases.”
Firefighters in Los Angeles were among the first of essential workers/healthcare workers to receive the FDA-approved vaccine on December 27.
As of 2:39 PST, December 30, 8,665 deaths and 113,364 cases were reported in California by the LA Times. CNN reported at 5:02 p.m. EST that some 2.2 million US citizens were vaccinated, while the goal for the end of the year had been 20 million.
The new COVID variant first detected in the United Kingdom, perceived to be more contagious, with the New York Times estimated it to be some 50 percent to 70 percent more contagious, as identified on that day in Southern California and Colorado.






